Our Services
Orthotic And Insole Therapy
Orthotic therapy, otherwise known as insole therapy is a form of treatment that Podiatrists can use to manage a variety of complaints. Orthotics are devices that are designed to sit inside your footwear and interact with the foot. This interaction has a direct influence on the body, affecting posture, balance and function. They come in a wide variety of forms, shapes and materials, each having a particular use.
At Fluid Movement Podiatry, we specialise in the assessment and prescription of orthotics to assist our patients. Each patient functions differently and therefore needs different requirements to assist in their normal day-to-day life. Whether this be with sport, balance improvement, injury management, pressure distribution and/or rehabilitation, orthotic needs can vary enormously.
As part of our service, we look holistically at each patient’s function. This involves assessing how the foot, lower limb, knees, hips and lower back function together. This process is known as a biomechanical assessment. Simply, a biomechanical assessment reviews the way you move relative to your problem and aims to establish areas of weakness or high stress so that we can build a plan that will normalise the stress or weakness. This assessment allows us to best identify the most appropriate form of treatment required and whether orthotic therapy will be of benefit.
Orthotic treatments are tailored to the individual and range from firm, semi-flexible and soft insoles. They can be functional in their role, therefore influencing joint stress or muscle function. They can also be palliative in their role, thus reducing pressure on an area of the foot that is susceptible to break down or ulceration, like in a person with diabetes. Insoles can be custom-made to suit your foot and specific condition and we also stock a large number of pre-manufactured insoles that we can modify and mould to suit your treatment needs.
Orthotic therapy is generally only one part of the overall treatment plan. Orthotics can certainly bring about improvements on their own, however they are best complimented with other forms of treatment. When we involve a variety of forms of treatment in your management plan, we usually see more rapid changes in comfort and a greater ability to ensure long lasting benefits.
Common complimentary therapies that we at Fluid Movement Podiatry use along side orthotic therapy are:
- Dry needling
- Massage therapy
- Injection therapy
- Strapping techniques
- Padding techniques
- Stretching – passive and active
- Mobilisation
- Exercises – to improve muscle function, balance and movement patterns
- Footwear modification and advice
- Re-introduction to normal day-to-day or sporting activities – rehabilitation
“I like to think of an orthotic as a type of aid. They may not necessarily perfect someone’s alignment however they are a tool that can be used in a variety of circumstances and age groups with good effect.
They can be used to alter stress across a certain joint, muscle or tendon to normalise the stress. This can help with recovery from an injury or be used as a way of helping prevent injury in the future. Also they are often used to manage load on a certain area of your foot to improve weight-bearing distribution. This can assist with improvements in balance and help prevent falls and also help manage the consequences of higher foot pressures, such as corns and calluses.
While in the UK, I worked with a large number of people who suffered from hip and lower back concerns, mainly chronic. Assessing how the feet interact and influence the rest of the body can give us great insight into how to stabilise some of these concerns. Managing a patient’s function from a foot and lower limb perspective can dramatically improve loads through their knees, hips and lower back. It can allow a patient to improve day-to-day comfort and help them progress their rehabilitation or exercises therapy.
Orthotic therapy is often best complimented with other therapies. These can further enhance the orthotic benefits and aim at ensuring long-term effect. Complimentary therapies can include exercises, massage, dry needling, stretching and activity modification.”
Ben Millerd – Podiatrist
B.Pod. B.Hlth Sc. (Human Movement)
M.A.P.A

Diabetes Management
At Fluid Movement Podiatry we are actively involved in the assessment, management and treatment of those who have been diagnosed with Diabetes.
Diabetes can have a broad effect on the body as a whole, and in particular the feet. It is important to have a thorough Diabetes foot assessment on a regular basis to ensure your ongoing foot health. People with Diabetes are more at risk of complications, including nerve damage and circulation impairment.
At Fluid Movement Podiatry we will undertake a detailed assessment, which reviews:
- Vascular status (blood flow/circulation)
- Neurological status (nerve sensation in the feet)
- Skin health
- Nail health
- Footwear assessment
- Weight-bearing assessment (balance and foot pressures)
- Ongoing education
As part of the overall and long-term management of our patients, we provide feedback and assessment results to your doctor’s and other health care professionals to keep everyone informed and ensure a more holistic health care program.
Prevention is the key to the long-term management of any diabetic foot complications. Therefore, early detection through regular check-ups is one of the vital ways to ensure your feet and body stay healthy and active.
Please feel free to contact the practice for further information on the role we can play in the management of Diabetes.
Further reading can be found at:

Corrective Nail Surgery
Ingrown toe nails are a common problem. They are painful, unsightly and often expose you to a greater risk of infection. If treated early, an ingrown toe nail can end up being a very minor issue which clears up without any ongoing concern. However, for some people this issue can become a chronic problem. Quite often these people have had some form of trauma to their nail, which may have been caused by abnormal pressure from different footwear, playing sport, poor cutting technique or simply an involuted (very curved) nail that is difficult to manage. In these cases, further intervention/treatment may be required to ensure the problem is addressed both in the short and long-term.
Corrective nail surgery is a minor procedure performed under local anaesthetic. It generally involves the removal of the small problematic section of nail, to ensure long-term comfort is achieved as well as retain the overall aesthetics of the remaining nail.
This procedure is generally referred to as a Partial Nail Avulsion, however in very extreme cases we have to remove the whole nail, which is referred to as a Total Nail Avulsion.
If you would like to know more or determine your suitability for the procedure please contact the clinic.

Functional Analysis / Biomechanical Assessment
A big part of our passion at Fluid Movement Podiatry is the analysis of the body as a complete unit. We are fascinated how all the joints, muscles and parts of the body relate and in particular work together. This form of assessment is called a biomechnical assessment. Given the foot is only one element of the amazing body system we have, we need to look at the body as a holistic structure to ensure we identify the cause and can determine the most specific treatment options for our patient’s root problems’. By taking a holistic approach at Fluid Movement Podiatry we are better equipped to diagnose and treat conditions to ensure a long-term benefit rather than just a short-term fix.
Biomechanical assessments involve a number of key elements and tests that are used to obtain a clear overview of the body’s movement behaviour, restrictions and possible compensations that are taking place. The results of a biomechanical assessment are used to generate a diagnosis and treatment plan. The different elements that make up a thorough biomechanical assessment include:
- Joint range of motion testing
- Muscle strength testing
- Static postural assessment
- Dynamic assessment (walking/running analysis)
- Functional testing (review the body’s ability to perform certain movements)
- Flexibility testing (muscle elasticity)
When you come to see us it’s a great idea to bring a pair of shorts to allow us to assess your mechanics efficiently.

Heel pain Management
Heel pain is one of the most common foot complaints that people will experience in their life. There are numerous conditions that can cause heel pain, however the most common effects the base of the heel area and is often referred to as plantar fasciitis. This condition will affect roughly around 1 in 10 adults at some stage in their life.
The plantar fascia is a ligament-like structure that runs from the base of the heel bone to the ball of the foot. It acts to support the structure of the foot, especially when walking and standing.
It is often highlighted by pain under the heel and sometimes into the arch area of the foot. A lot of people will be first aware of it after getting out of bed in the morning. They will place their foot down on the floor and feel instant pain and discomfort, finding it difficult to walk. This often eases as the person spends a little longer on their feet or after a shower, as the fascia starts to warm up and improve its general elasticity. The pain can often return through the day and be achy of an evening depending on the person’s level of activity throughout the day.
Prominently, this type of heel pain can arise by an increase in stress/strain on the feet. This could include a sudden increase in activity levels, changes in footwear, increased weight gain, prolonged standing and muscle stiffness as common factors.
Heel pain can often become a more chronic issue for people as the feet are such an important part of most people’s lifestyle to get from A to B or just undertaking everyday activities.
The first step in management is a careful review of your history to ensure a proper diagnosis is made. This also allows for a more specific treatment and management plan to be formulated for each specific case. Everyone lives a different lifestyle and moves in their own unique way, so identifying the main factors that could have contributed to the complaint are vital to determining the best course of treatment.
Heel pain management must be comprehensive to improve pain levels and to allow the individual to return to their normal level of activity as soon as possible.
Management often involves initially reducing the load on the heel and plantar fascia. This can be achieved via a variety of ways:
- Strapping and padding
- Footwear review and recommendations
- Massage, mobilisation techniques
- Orthotic or insole therapy
- Dry needling – myofascial trigger points
- Stretching
- Modification of aggravating activities
One of the key things to long term resolution of this condition is to address strength and flexibility of the muscles in the foot and legs, along with the fascia itself. Once the pain and person’s tolerance has improved with initial management it is important to promote and restore strength and function to the lower extremity. A plan will be made to suit your needs and managed at the appropriate time.
There are though, unfortunately people who will have a more difficult time with their heel pain. They may progress very slowly or have more significant pain that can make it very difficult to even get through the day. These people will be managed appropriately and may require other treatments to assist in their pain management. Some further treatments may involve:
- Shock wave therapy
- Cam walker – immobilisation boots
- Cortisone injections
- Prolotherapy – Injection therapy – to promote healing
Shock wave therapy is a specialised treatment that can be very effective for chronic heel pain suffers. Fluid Movement Podiatry uses shock wave therapy in a variety of ways to help with pain management, promote healing and improve mobility of the muscles around the foot and leg. We have a long history of using this modality to the benefit of our patients. Please feel free to read further about how Shock Wave therapy could assist you.
Even though the plantar fasciitis may be the most common issue related to heel pain, there can be a vast variety of other issues which effect the heel of the foot. Each of these have various symptoms and presentations, therefore a thorough assessment is important. Some of the more common issues that can also effect the heel are:
- Nerve entrapment
- Heel bone fracture/bruising
- Fat pad irritation
- Tarsal Tunnel Syndrome
- Cyst formation
- Systemic Inflammatory conditions
- Achilles issues
- Inflamed Bursa

Shock Wave Therapy
What is Radial Shockwave Therapy?
Radical shockwaves are high-energy sound waves, or otherwise known as acoustic shockwaves, which are transmitted through the skin into the underlying tissues. This helps to breakdown stiff/rigid tissue, increases blood flow and stimulates tissue repair. Essentially it kick starts the body’s natural healing mechanism.
Radial shockwave therapy is most commonly used for treatment of chronic musculoskeletal conditions that are not responding to conventional treatment, most commonly plantar heel pain (Plantar fasciitis) or achilles tendinopathy
What Does a Radial Shockwave Therapy Session Involve?
Radial Shockwave therapy is a safe, non-invasive procedure. A contact gel is applied to area of application, then a handheld probe is applied to the skin. The probe delivers the acoustic waves in a controlled and focused manner for typically a 5-minute period to the injured site
What Does a Course of Radial Shockwave Therapy Session Involve?
A course of shock wave therapy usually consists of 3-5 sessions. This is ideally performed 1 week apart for optimum results. If a condition is more chronic or significant in nature, it’s more likely a 4-5 session course will be required
Will other therapies be helpful while having Radial Shockwave Therapy?
The body is a complex structure and often an injury can have a number of factors that can influence pain and healing. You will have your problem assessed to determine the best approach for your condition. It will often involve a combination of therapies to best improve pain and mobility while undertaking Radial Shock Wave Therapy

Forefoot Issues
The forefoot is one of the more common areas of foot complaints seen by a podiatrist.
The forefoot is a complex area made up of a number of bones surrounded by nerves, ligaments, muscles and tendons all packed in a tiny little area.
Given how much we are on our feet everyday with our everyday activity, work and exercise, this area is subject to a huge amount of load.
Usually the body is very good at dealing with this amount of pressure and stress. However, certain factors can increase the stress on the forefoot area resulting in pain and injury. Some of these include:
- Prolonged periods standing or walking
- Sudden increase in activity
- Improper fitting footwear – particularly shoes that are too small
- High intensity activities – running and jumping sports
- High heeled shoes put extra pressure on the forefoot
- Structural foot issues – bunions or hammer/claw toes
- Foot biomechanics – high arched or flat feet
- Hip and knee issues – can change walking pattern
- Tight/weak calf muscles
- Fat pad atrophy
- Medical conditions:
- Gout
- Osteoarthritis
- Rheumatoid arthritis
- Diabetes
Some common forefoot conditions we see and treat include:
Morton’s Neuroma:
Morton’s neuroma involves a thickening of the tissue surrounding the nerves running between the toe joints on the ball of the foot. Symptoms may include a burning pain that starts in the ball of the foot, running into the toes. You may also experience feelings of numbness or tingling in the area, or feeling like you are walking on a pebble. This is most common between the 3rd and 4th toes
Intermetatarsal Bursitis
Symptoms for Intermetatarsal bursitis may be similar to those of a Morton’s neuroma. This is because both conditions can influence the small space between the toes where the little nerve branches run.
Bursitis is an inflammation of small fluid filled sacs called bursa. This often presents with some mild swelling across the forefoot. This increased swelling often leads to pressure on the nerve which can cause mild nerve like symptoms in the area and into the toes.
Bunions
Bunions are a relatively common foot deformity, which have a strong genetic predisposition. They are characterised by a visible bump and deviation of the big toe away from its original position.
This can make finding correct fitting footwear difficult and in certain cases, may result in pain. There is often joint degeneration of various severities associated with the formation of a bunion.
If the deviation of the big toe is great enough, this may also effect the lesser toes causing them to curl up to accommodate the movement of the big toe.
There is a variety of management strategies that can be used to improve comfort and function in most cases.
Hammer/Claw Toe:
Hammer or claw toes are deformities that cause your toes to curl and bend down instead of pointing straight forward.
These toes can cause excess pressure and rubbing, especially in small or narrow fitting shoes.
Plantar plate injury:
The plantar plate is a fibrocarilaginous structure lying directly underneath the joints on the ball of the foot. One of its main roles is to help stabilise the metarsophalangeal joints (the knuckle like joints just before your toes start) to help keep the toes straight and inline with each other.
Symptoms of a plantar plate injury may include pain or swelling on the top or bottom of the forefoot joint (Most commonly the 2nd toe). In some cases the affected toe may start to lift up in the air or creep across to the side.
Sesamoiditis:
Sesamoiditis involves pain and inflammation underneath the big toe joint. Underneath the joint are two small bones called sesamoids, these help the toe to function more efficiently.
Certain activities, footwear types or biomechanical abnormalities can increase the load on these tiny bones causing them to become inflamed and painful.
Symptoms may include pain directly underneath the big toe made worse by walking or wearing thin soled or high-heeled shoes.
Stress Fractures:
Stress fractures are tiny cracks in the bone. They are often caused by repetitive overload of a bone in the foot most commonly the 2nd and 3rd metatarsal bones.
The main complaint of stress fractures is pain with activity. This may start as mild but get worse over time, most often aching even at rest. There may be swelling, bruising or significant tenderness at a specific area.
Osteoarthritis
Osteoarthritis can affect all joints in the forefoot, with the most common being the big toe joint. Symptoms of arthritis may include pain, swelling or joint stiffness, often worsening over time. In sever cases this pain may start to become more constant even becoming painful at night while at rest.
Corns and Callus
Corns and calluses are simply areas of hard, thick skin on the feet. Once this skin becomes too thick it can become very painful to walk on. Luckily can be very easily removed by your Podiatrist. For more information, please feel free to see General Foot Care link.

Rehabilitation
“The human foot is a masterpiece of engineering and a work of art”
Leonardo Da Vinci (1452 – 1519)
We cannot agree more. It’s a complex piece of engineering which has to absorb shock, balance and stabilise the body. It helps hold us upright but also works to propel us forward, all while taking some of the highest loads of any part of the body. They have to work with a whole chain of muscles to continue to perform basic movements we often take for granted. Our feet and legs are often given very little attention, until something does go wrong.
Unfortunately, things can go wrong and things can be injured through overuse, a sports injury or even alter its function as a result of conditions like arthritis or following surgery.
Each of these complaints or injuries influence the tolerance and capacity of the foot and legs. Often we will compensate to manage but long term this can bring with it more significant issues which can affect other parts of our bodies especially the back, hips or knees.
Ensuring we restore appropriate movement patterns, muscle strength, balance and mobility is vital to ensure no further injury is developed and we are able to return to our level of activity we so desire.
This is where rehabilitation is a big part of treating our patients. We are known for not only managing our patients’ complaints/injuries but also ensuring they return with appropriate function.
We have a strong background in exercise prescription that is very unique to managing loads on the feet and legs. As outlined they need to do a lot but sometimes we have to be very particular about how we strengthen and load different muscles, joints etc as they are very easily overloaded. When we overload things they very often will struggle to recover and bring with it pain and sometimes inflammation. Repeated inflammation can delay the healing response and thus hinder a person’s progress. This is where we will support you with a very specific and guided plan to ensure you have clarity on what to do at the various stages of your rehabilitation.
Post- Surgical Rehabilitation
One of our areas of interest is helping people return from foot and ankle surgery. We can help with the return of mobility and function and guide you through this period, which can often be challenging. Surgery is usually required to manage various complex issues that conservative therapy may not. However, often recovery from surgery initially involves immobilisation, thus a loss of strength and flexibility follows. The challenge is often people have had to compensate prior to actually having the surgery. They may have altered their walking pattern, balance and used other muscles to protect the area that may require surgery. Therefore, this means that not only do they have weakness following immobilisation from surgery, they very likely have not walked efficiently for some time.
This can become a complex situation as post-surgically people will try and return to their normal movement behaviour, however will not necessarily have the strength or flexibility to achieve this.
Some muscles are quick to adapt, while others are much more particular and will need more gradual loading. A thorough assessment of someone’s ability to engage muscles, their strength, flexibility is important. A broader look at how someone uses the muscles around their hips, and legs is also important to helping our patients return to more comfortable movement. This focus has a greater global effect on the body and better addresses our patients long term return to optimal function.
Please feel free to contact us if you have any questions related to rehabilitation or a specific complaint that you may want to gain more information about how we could assist.

Sports Injuries
Here in Melbourne we love our sport, with a wide range of athletes from the weekend warrior to those a little more serious. We can’t get enough of it!
Unfortunately, one thing that can come with playing sport, are injuries. They can happen when we least expect it, with a more sudden incident, or actually gradually develop over time and frustrate an athlete.
Luckily here at Fluid Movement Podiatry we have a particular interest in assessing, diagnosing and treating all sporting and running related injuries.
We have a long history in assisting our patients identifying the issue at hand and helping them with the short and longer term management of these injuries.Common sporting injuries we see and treat:
- Ankle sprains – both acute and chronic issues
- Medial tibial stress syndrome (Shin splints & other issues)
- Achilles pain
- Arch and heel pain
- Forefoot pain
- Lower leg muscle and tendon pains
- Patellofemoral joint pain (Knee pain)
- Stress fractures
- Hard skin management
- Toenail injuries
The load on our feet and legs during sporting activities can be quite significant and often many of these injuries result from variation in training loads, muscular and/or postural imbalances.
As part of your management we will spend time looking at these issues, working through your training/activity history and clinical assessments to identify all factors that may have led to your injury.
We will then work with you, taking into account your exercise and fitness goals to developing a specific tailored management plan. As part of this plan will also involve a rehabilitation program to get you back on track in the shortest time possible.
Feel free to contact us if you have any questions about a complaint or injury that you may have.

Dry Needling
What is dry needling?
The process of dry needling involves inserting extremely thin, sterile needles into very tight areas of the muscle known as Myofascial trigger points.
How does it work?
Myofascial trigger points are characterised as taught sections of the skeletal muscle or fascia (If you have a feel around your calf now I’m sure you can find some!).
Pressing on these points may elicit a local or referred pain or in some cases even a slight twitch response of the muscle.
When the needle is inserted into these trigger points, the muscle around the needle begins to relax. This can help to reduce the tension within the muscle, improve pain, range of motion and even muscle function.
Dry needling can be a very effective method of easing pain and tension within a tight muscle. It should be noted though, this technique is often used in conjunction with other treatment modalities such as exercise, load management, taping or footwear modifications.
For more information or to see if you are suitable for dry needling contact one of our Podiatrists today.

General Foot Care
Sometimes what seems to be a small problem can often be the most annoying. We are also conscious that a small problem can in turn cause a bigger problem if left unattended.
Fluid Movement Podiatry are therefore very particular about addressing these problems not matter how small they may appear. We recognise the importance of general foot care as an integral part of maintaining our patients comfort and mobility.
Our feet are constantly involved in dealing with pressure and stress every day. The average person can walk as much as 4 times around the earth in a lifetime. That is a lot of work!
When we place repeated load on the feet it can cause friction and pressure across the foot. The body often responds by increasing the thickness of the skin, therefore producing calluses and/or corns. The consequence is the skin loses its natural elasticity. This can cause discomfort and restrict normal blood flow to the foot. It is very important to those who have been diagnosed with Diabetes but also to the average person. We at Fluid Movement Podiatry offer general foot care for anyone who may have difficulty in attending to their own foot health. Comfortable feet are important for ongoing mobility and falls prevention. We offer a comprehensive service to ensure you get the right advice and treatment to keep you on your feet.
Common conditions we regularly treat are:
- Ingrown toe nails – ( further reading ‘Corrective Nail Surgery‘)
- Thickened or irregular nails
- Discoloured nails
- Involuted nails – very curved shaped nail
- General Toenail care
- Corns
- Calluses
- Chill blains
- People with Diabetes (Further reading Diabetes Management)
- Skin complaints (fungal/tinea, psoriasis, hyperhydrosis, pitted keratolysis, etc. )
- Warts (Verruca pedis lesions)
- Skin break downs (ulcerations)
- Blisters

Children’s Feet
Young feet can range from babies to older teenagers. They all develop in their own unique way, and in their own unique time frame. However, sometimes young feet can develop pain or other concerns which can interfere with their ability to play freely.
Common conditions we see and treat are:
Flat Feet
The foot will gradually develop, with the muscles and ligaments of your foot strengthening to form some form of arch. Between 0 and 2 years your child’s feet will appear flat, this is very normal in a young child due to the natural way the foot is developing. When your child begins walking, muscles and bones will strengthen and help form their longer term foot posture. This often presents with a more obvious arch contour, but sometimes this may not be the case. There is obvious variation with every set of feet, but if you have any concerns or there is a family history of flat feet, a simple check-up may be all that is required to identify if this is within normal limits or not.
In-Toeing
Many toddlers appear to be walking like they are ‘pigeon-toed’, or have feet that turn inwards. In most cases, this is a normal part of your child’s developing posture and alignment. This should start to naturally straighten between the ages of 3 and 6. However, if there is a concern that this is not improving, one is more pronounced than the other foot or you are starting to notice your child tripping or getting tired when active, it’s a great time to see us to have a more detailed look into its presentation. Assessment will often determine the extent, where it is coming from and allow for appropriate management if required. The great thing is the majority of in-toeing feet improve as the child matures.
Severs and Heel Pain
Severs is a common complaint that often affects very active children. It results from the inflammation/irritation of the growth plate in the heel bone. Severs usually occurs during periods which we often call ‘growth spurts’. Girls between the ages of 8 and 13 are likely to experience it, while it is more common in boys between 10 and 15 years of age. There are numerous factors that can contribute to your child experiencing pain in their heels. It is therefore, important to have this assessed by your podiatrist to ensure things are identified early.
Toe-walking
Is where the child has limited if any heel contact with the ground while walking. The great thing about this is it is rather normal for children under the age of 2-3 years of age.
Toe walking is often just a part of a child’s developmental phase. However, it can also indicate other underlying conditions. As part of our thorough assessment we will be able to identify the true nature and assist you with a greater understanding or your child’s development.
Other conditions
There are many other conditions and developmental concerns that can affect young people’s feet and legs. Warts, knee pain, arch pain, shin pain, nail concerns, including in-grown toenails are just a few of the other conditions we see.
There are far too many to elaborate on, however be assured our detailed assessment of each child’s concerns will always be our initial focus.
How do our Podiatrists assess Children’s Foot Problems?
Finding the cause of your child’s foot concern requires detailed assessment.
This will include:
- a thorough birth and developmental history;
- history of symptoms;
- full biomechanical assessment (including gait that is age appropriate);
- neurological assessment (nervous system); and
- footwear assessment.
- Skin or nail health assessment (as required)
By conducting a thorough assessment of your child’s feet, your Podiatrist can ensure that a suitable treatment plan is provided.
It is important to note that not all children’s concerns require intervention. Sometimes it’s just the natural developmental phase for your child. We are here to assist in helping you get the best advice and information so you are fully informed.

Professional CAM Walker Fitting
You may have seen people walking around in a moon boot. These are actually called CAM walkers or Controlled Ankle Motion walkers often referred to as “moon boots”. CAM walkers are used to minimise movement at the foot and ankle. They also significantly reduce the load and forces placed on the bones, joints, tendons and muscles.
At Fluid Movement Podiatry we stock a full size range of CAM walkers and other orthopaedic immobilisation devices, to help you recover as quickly as possible from an injury. We provide a professional fitting service for all types of foot and ankle injuries. We will ensure your boot fits properly and can make on the spot modifications to get the best fit. We will help you gain confidence in using the boot correctly so you get the most benefit from it.
CAM walkers are a great tool for a variety of conditions particularly acute fractures and severe ankle sprains. They can also be useful for a range of other conditions. Occasionally, a CAM walker is needed for a few weeks to calm down an injury that is highly irritable. Sometimes an injury is just too painful to respond to normal treatments. A short period in a CAM boot can allow it to settle enough to gain momentum with rehabilitating your injury.
Below are some common conditions CAM walkers can be used for:
• Fractures
• Stress fractures
• Ankle sprains – in sever cases
• Post surgical recovery
• Plantar heel pain – in sever cases
• Non-responsive tendinopathies
• Tendon ruptures
• Diabetic foot ulcers
How long do I need to wear it?
We will advise you on how many weeks to use your CAM walker. This will depend on the type and severity of your injury. For non-complex fractures this will generally be between 4-8 weeks however this can vary depending on the location and type of fracture.
Do I need to use crutches?
You may have seen some people using a CAM walker and crutches. Generally, crutches are used in addition to a CAM walker in the very early stages of healing after a fracture or following surgery. For most other injuries crutches are not required, however we will assess your injury to help determine whether crutches are necessary.
What activities can I do in a CAM walker?
This will vary depending on the condition being treated. The idea of the boot is to offload your injured tissue/bone and allow it to recover. We recommend you minimise walking where possible. We can guide you on alternative forms of exercise. We regularly prescribe home exercise programs to help minimise de-conditioning in the hips, knees, foot and ankle that can occur while you are wearing your CAM walker.
Do I need to wear it all day?
You will need to wear your CAM walker for all weight bearing activities. For the fastest recovery you will need to wear at all times. If you are working from home or have a desk-based job, you may not have to wear it while you are sitting at your desk. We can discuss your individual circumstances with you during your fitting appointment.
Are there other options?
Yes. While CAM walkers are extremely effective because they limit movement across the ankle joint, they are not the only option. In some cases, a below ankle device, which allows the ankle to bend may be preferable. We can help guide you on the best treatment options for your injury.
The image below shows a ‘post-op shoe’. This device is stiff soled, lightweight and easy to use below ankle device. It is a great option to offload an injury within the foot that does not require restricting movement at the ankle.
We can assess your injury to determine whether you can use a post op shoe or a CAM walker.
Below are some common injuries that a post op shoe can be used for include:
Specific fractures or stress fractures
Sprains or ligament injuries in foot (such as turf toe)
An aggravated joint
Following forefoot surgery
Toe or forefoot injuries
Do I have to buy my own CAM walker?
Yes. You can buy your CAM walker directly from our clinic. Your CAM walker will become your new best friend and you will need to wear it daily for a number of weeks. We will help fit your boot to cater to your individual needs. We don’t hire out boots as they are often required for many weeks and become slightly moulded to your foot and ankle structure.
I am out of the boot! Now what!?
Once your fracture has healed or your pain level has improved, we will guide you through the next phase of your rehabilitation. It is normal to lose some strength and conditioning after wearing a CAM walker. We can help you return to your normal activity using our expertise in sports injury and rehabilitation.
If you think you might need a CAM walker, we can help ensure you get the best fit and guide you through your rehabilitation.

Richie Brace
A Richie brace is a customised ankle brace that combines both a custom foot orthotic with above ankle support. It provides a greater level of stability compared to a traditional orthotic. It is used to help stabilise the foot and ankle and has great applications for a variety of conditions. The Richie Brace is often used in those who may not have responded to other treatment options and are keen to avoid surgery or keep moving as long as possible.
Richie braces are very effective for conditions known as adult acquired flat foot disorder. In this instance a traditional orthotic may not provide adequate support and a Ritchie Brace can used to provide greater stability and efficiency for the individual to control pain and improve mobility..
At Fluid Movement Podiatry we specialise in fitting and prescription of Richie Braces. We have helped many people suffering from foot and ankle issues with varying levels of complexity. We use Richie Braces as both a short term and long term treatment option. In short term instances it can used effectively to help return somebody to their normal level of activity. Ritchie braces can also have long term applications to help patients avoid foot and ankle surgery.
Richie Braces are customisable and can be used for all daily activities including walking, running and your desired activity or sport. We take into account your requirements and activities when prescribing the device.
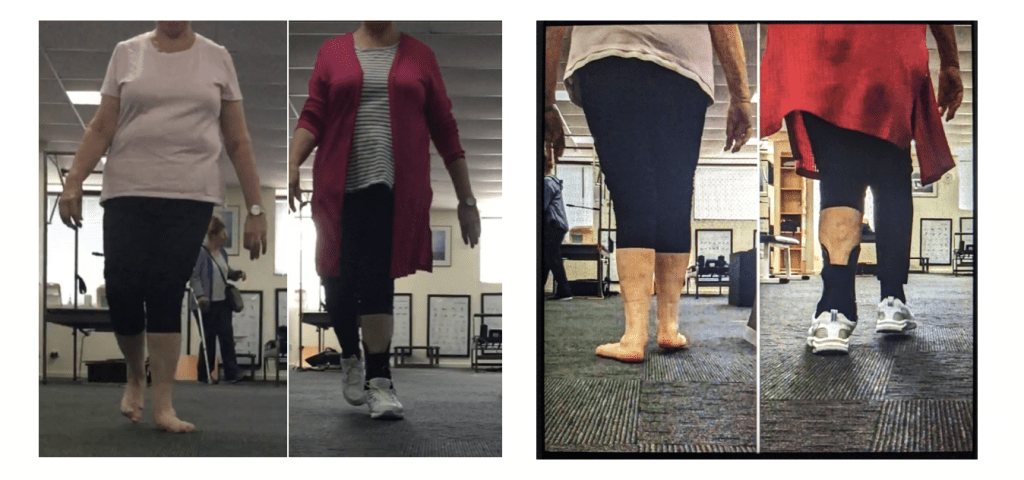
Actual case at Fluid Movement Podiatry:
The below images were taken from one of our many patients we see with rather complex foot and leg issues. Often the influence of these complex foot and ankle issue can have detrimental effects on the hip, knee and lower back. Often in cases like this, there is a noticeable hip drop when the patient walks. They will generally suffer from hip, knee or lower back pain as they have to compensate from the changes in at the foot and ankle. This is the value in the use of a Richie Brace; it can influence all these structures to improve balance and function and pain.
In this photo you can see the complete loss of arch on the left foot and the effect on the position of the knee and the hip. In this instance a traditional foot orthotics is not able to provide adequate support to the foot. The Richie brace is required to provide the appropriate support above the ankle to also influence the knee, hip and lower back structures. function.
Another use for Richie Braces is a condition called chronic ankle instability. This condition typically develops gradually in someone which a high arch foot type who suffers from repeat ankle sprains. Eventually the foot ends up in an unstable position. The muscles that support the outside of the ankle are fatigued and at mechanical disadvantage due to the position of the foot. The image below shows that some people also suffer with the opposite to a flat foot (sever pronation) that forces their foot and ankle to the outside. This condition also has its own knee, hip and lower back compensations and can often cause pain or issues at these levels. A Richie brace maybe required to assist these individuals as a traditional orthotic is inadequate to manage and influence the foot and ankle enough for more optimal function and pain reduction.
Richie Braces are an excellent modality, especially for those with complex foot and ankle pain that is often long standing or may be considering surgery. At Fluid Movement Podiatry we provide specialist prescription and fitting of Richie Braces following a thorough assessment. Our aim is to minimise pain and improve balance and function. This can be for short term management or in some case can be used longer term. Please contact us if you have any questions.